Revenue Cycle Management (RCM) is a critical component of the healthcare industry, encompassing the entire financial process from patient registration to the final payment of services rendered. It involves a series of steps that ensure healthcare providers receive timely and accurate reimbursement for their services. RCM services are designed to optimize the financial performance of healthcare organizations by managing the flow of revenue through various stages, including patient scheduling, insurance verification, billing, coding, and collections.
Understanding RCM is essential for healthcare providers to navigate the complexities of reimbursement and maintain financial health. The importance of RCM cannot be overstated, as it directly impacts a healthcare organization’s bottom line. Inefficiencies in the revenue cycle can lead to significant financial losses, affecting not only the organization’s profitability but also its ability to provide quality care.
By implementing effective RCM strategies, healthcare providers can enhance their operational efficiency, reduce costs, and improve patient satisfaction. A well-managed revenue cycle ensures that healthcare organizations can focus on delivering high-quality care while maintaining financial stability.
Key Takeaways
- Effective Revenue Cycle Management (RCM) integrates billing, coding, patient registration, and claims submission to optimize healthcare revenue.
- Leveraging technology and data analytics enhances accuracy, reduces denials, and improves overall RCM performance.
- Streamlined patient registration and insurance verification are critical for minimizing claim rejections and delays.
- Compliance with regulatory requirements and payer policies ensures smooth reimbursement processes and reduces risks.
- Outsourcing RCM services can provide cost-effective solutions while continuous evaluation of ROI drives ongoing improvements.
Implementing Effective Billing and Coding Strategies
Billing and coding are fundamental aspects of RCM that require precision and expertise. Accurate coding ensures that healthcare services are correctly represented in claims submitted to insurance companies, which is crucial for receiving appropriate reimbursement.
Regular audits and updates to coding practices can help identify areas for improvement and reduce the risk of errors that could lead to claim denials. Moreover, effective billing strategies go beyond just coding accuracy; they also involve optimizing the billing process itself. This includes establishing clear communication channels between clinical staff and billing departments to ensure that all necessary information is captured at the point of service.
By streamlining the billing process and reducing administrative burdens, healthcare organizations can enhance their revenue cycle efficiency and minimize delays in payment. Investing in ongoing training and development for billing staff is essential to keep pace with the ever-evolving landscape of healthcare regulations and payer policies.
Leveraging Technology for Streamlined RCM Processes

In today’s digital age, leveraging technology is paramount for streamlining RCM processes. Advanced software solutions can automate various aspects of the revenue cycle, from patient registration to claims submission, significantly reducing manual errors and improving efficiency. Electronic Health Records (EHR) systems integrated with RCM tools can facilitate seamless data sharing between clinical and administrative teams, ensuring that all relevant information is readily available for billing purposes.
This integration not only enhances accuracy but also accelerates the overall revenue cycle. Additionally, technology can provide valuable insights through data analytics, enabling healthcare organizations to identify trends and areas for improvement within their revenue cycle. By utilizing predictive analytics, organizations can forecast cash flow, assess the likelihood of claim denials, and make informed decisions about resource allocation.
Implementing a robust RCM technology platform can empower healthcare providers to optimize their processes, enhance patient experiences, and ultimately drive revenue growth.
Optimizing Patient Registration and Insurance Verification
| Metric | Description | Target Value | Current Value | Improvement Strategy |
|---|---|---|---|---|
| Average Registration Time | Time taken to complete patient registration | 5 minutes | 8 minutes | Implement digital forms and pre-registration |
| Insurance Verification Accuracy | Percentage of insurance verifications completed without errors | 98% | 90% | Use automated insurance verification software |
| Patient Wait Time Before Registration | Average wait time patients experience before starting registration | 3 minutes | 7 minutes | Schedule appointments with buffer and optimize staffing |
| Claim Denial Rate Due to Registration Errors | Percentage of insurance claims denied due to registration mistakes | 2% | 6% | Staff training and real-time data validation |
| Percentage of Pre-Verified Insurance | Proportion of patients whose insurance is verified before arrival | 85% | 60% | Implement online pre-verification portals |
| Patient Satisfaction Score | Patient feedback rating on registration process (scale 1-10) | 9 | 7 | Streamline process and improve communication |
The patient registration process is the first step in the revenue cycle and sets the tone for subsequent interactions. Optimizing this process is crucial for ensuring accurate patient information is collected upfront, which can significantly impact billing and reimbursement. Healthcare organizations should implement user-friendly registration systems that allow patients to provide their information easily, whether online or in-person.
Training staff to verify insurance eligibility at the time of registration can also help prevent issues later in the revenue cycle. Insurance verification is another critical component that requires meticulous attention. Ensuring that patients’ insurance coverage is verified before services are rendered can mitigate the risk of claim denials due to coverage issues.
Organizations should invest in technology that automates insurance verification processes, allowing staff to quickly confirm eligibility and benefits. By streamlining patient registration and insurance verification, healthcare providers can enhance operational efficiency and improve their chances of receiving timely payments.
Ensuring Accurate and Timely Claims Submission
Accurate and timely claims submission is vital for maintaining a healthy revenue cycle. Claims must be submitted promptly after services are rendered to avoid delays in payment. Healthcare organizations should establish clear protocols for claims submission, including timelines for submitting claims based on payer requirements.
Regular training sessions for billing staff on best practices for claims submission can help reduce errors and ensure compliance with payer policies. Moreover, implementing a robust claims management system can facilitate real-time tracking of claims status, allowing organizations to identify any issues early in the process. This proactive approach enables healthcare providers to address potential problems before they escalate into denials or delays in payment.
By prioritizing accurate and timely claims submission, organizations can enhance their cash flow and minimize disruptions in their revenue cycle.
Minimizing Denials and Rejections through Effective RCM Practices

Denials and rejections are significant challenges within the revenue cycle that can lead to substantial financial losses for healthcare organizations. To minimize these occurrences, it is essential to implement effective RCM practices that focus on identifying common denial reasons and addressing them proactively. Regularly analyzing denial data can provide insights into patterns that may indicate underlying issues within the billing process or documentation practices.
Training staff on proper documentation techniques is crucial for reducing denials related to insufficient information or coding errors. Additionally, establishing a dedicated team to manage denials can streamline the appeals process and improve recovery rates. By fostering a culture of accountability and continuous improvement within the revenue cycle team, healthcare organizations can significantly reduce the incidence of denials and enhance their overall financial performance.
Improving Payment Collections and Accounts Receivable Management
Effective payment collections are essential for maintaining a healthy cash flow within healthcare organizations. Implementing clear policies for patient payment responsibilities can help set expectations upfront, reducing confusion and improving collection rates. Offering flexible payment options, such as payment plans or online payment portals, can also enhance patient satisfaction while facilitating timely collections.
Accounts receivable management plays a critical role in ensuring that outstanding payments are collected efficiently. Regularly reviewing accounts receivable aging reports allows organizations to identify overdue accounts and prioritize follow-up efforts accordingly. Establishing a systematic approach to collections, including timely reminders and follow-up calls, can significantly improve recovery rates on outstanding balances.
By focusing on payment collections and accounts receivable management, healthcare organizations can enhance their financial stability and reduce reliance on external funding sources.
Enhancing Compliance with Regulatory Requirements and Payer Policies
Compliance with regulatory requirements and payer policies is a fundamental aspect of effective RCM practices. Healthcare organizations must stay informed about changes in regulations, such as HIPAA guidelines or Medicare reimbursement policies, to ensure they remain compliant. Regular training sessions for staff on compliance issues can help mitigate risks associated with non-compliance, which can lead to financial penalties or reputational damage.
Additionally, establishing a compliance monitoring system can help organizations track adherence to regulatory requirements and payer policies throughout the revenue cycle. This proactive approach enables healthcare providers to identify potential compliance issues early on and take corrective action before they escalate into significant problems. By prioritizing compliance within their RCM processes, organizations can safeguard their financial health while maintaining trust with patients and payers alike.
Utilizing Data Analytics for Performance Improvement and Revenue Maximization
Data analytics plays a pivotal role in enhancing RCM performance by providing actionable insights into various aspects of the revenue cycle. By analyzing key performance indicators (KPIs), such as days in accounts receivable or claim denial rates, healthcare organizations can identify areas for improvement and implement targeted strategies to optimize their processes. Leveraging data analytics allows organizations to make informed decisions based on real-time information rather than relying on historical trends alone.
Furthermore, predictive analytics can help organizations forecast future revenue trends based on past performance data. This foresight enables healthcare providers to allocate resources more effectively and develop proactive strategies for maximizing revenue potential. By embracing data-driven decision-making within their RCM processes, organizations can enhance operational efficiency while driving revenue growth.
Outsourcing RCM Services for Cost-Effective Solutions
Outsourcing RCM services has become an increasingly popular strategy for healthcare organizations seeking cost-effective solutions to manage their revenue cycles more efficiently. By partnering with specialized RCM service providers, organizations can leverage their expertise in billing, coding, and collections without incurring the overhead costs associated with maintaining an in-house team. Outsourcing allows healthcare providers to focus on delivering quality care while entrusting their revenue cycle management to experienced professionals.
Moreover, outsourcing RCM services can provide access to advanced technology solutions that may be cost-prohibitive for smaller organizations to implement independently. These service providers often have established processes in place that ensure compliance with regulatory requirements while optimizing revenue collection efforts. By outsourcing RCM services, healthcare organizations can achieve significant cost savings while enhancing their overall financial performance.
Evaluating the ROI of RCM Services and Continuous Improvement Strategies
Evaluating the return on investment (ROI) of RCM services is essential for healthcare organizations seeking to assess the effectiveness of their revenue cycle management efforts. Organizations should establish clear metrics for measuring ROI, such as improvements in cash flow, reductions in claim denials, or increases in collection rates. Regularly reviewing these metrics allows organizations to gauge the impact of their RCM strategies and make informed decisions about future investments.
Continuous improvement strategies are vital for ensuring that RCM processes remain effective over time. Organizations should foster a culture of innovation by encouraging staff to identify areas for improvement and share best practices across teams. Regular training sessions focused on emerging trends in RCM can also help keep staff informed about industry changes that may impact their work.
By prioritizing continuous improvement within their RCM efforts, healthcare organizations can enhance their financial performance while adapting to an ever-evolving landscape.
By implementing strategic billing and coding practices, leveraging technology, optimizing patient registration processes, ensuring accurate claims submission, minimizing denials, improving collections, enhancing compliance, utilizing data analytics, considering outsourcing options, and evaluating ROI through continuous improvement strategies, healthcare providers can navigate the complexities of the revenue cycle successfully.
Embracing these principles will not only safeguard financial health but also contribute to a more sustainable future in an increasingly competitive healthcare environment.
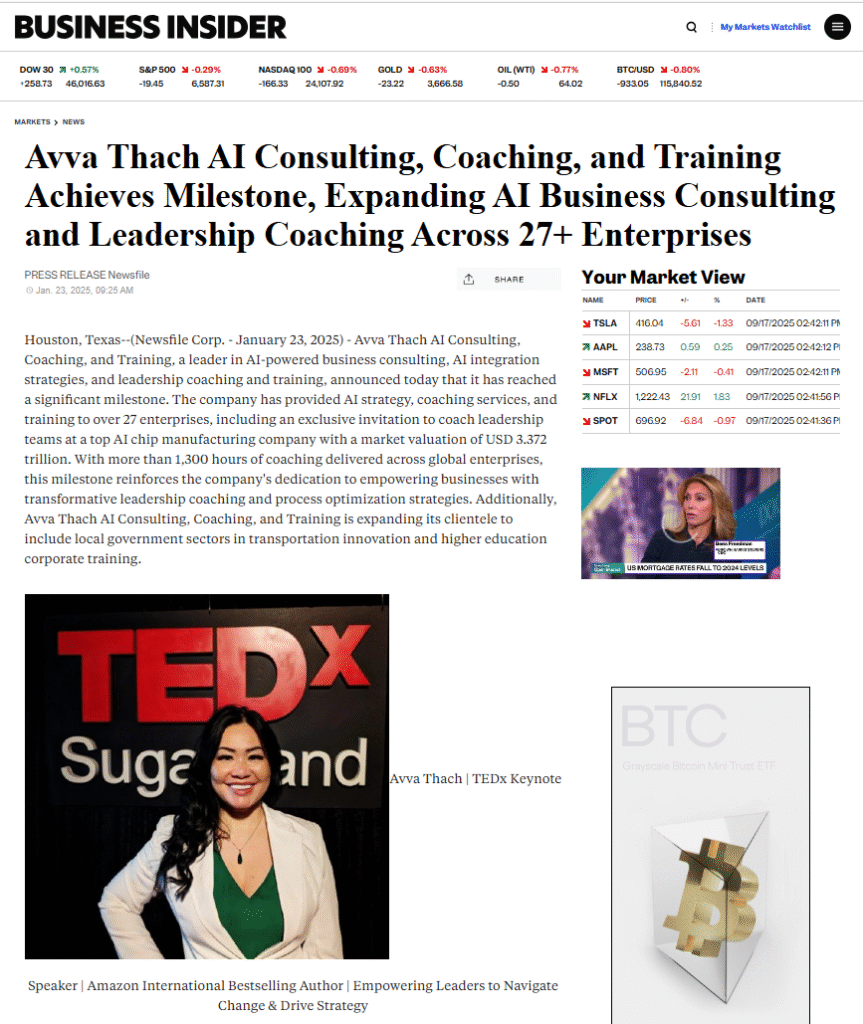
Revenue cycle management services are essential for healthcare organizations aiming to optimize their financial performance and streamline operations. For those interested in understanding how artificial intelligence can enhance business processes, a related article titled “Unlocking AI’s Disproportionate Returns: Shifting Focus to DPI” provides valuable insights. You can read it [here](https://iavva.ai/business/unlocking-ais-disproportionate-returns-shifting-focus-to-dpi/). This article discusses the transformative potential of AI in various sectors, including healthcare, and how it can be leveraged to improve revenue cycle management.
FAQs
What are revenue cycle management services?
Revenue cycle management (RCM) services refer to the process of managing the financial transactions and administrative functions related to patient care, from scheduling appointments to final payment collection. These services help healthcare providers optimize their revenue by streamlining billing, coding, claims processing, and payment collections.
Why are revenue cycle management services important for healthcare providers?
RCM services are crucial because they ensure timely and accurate billing, reduce claim denials, improve cash flow, and enhance overall financial performance. Efficient revenue cycle management helps healthcare providers focus on patient care while minimizing administrative burdens.
What tasks are typically included in revenue cycle management services?
Typical tasks include patient registration, insurance verification, medical coding, claim submission, payment posting, denial management, patient billing, and financial reporting. These tasks collectively ensure that healthcare providers receive appropriate reimbursement for their services.
Who provides revenue cycle management services?
RCM services can be provided by in-house billing departments, specialized third-party vendors, or healthcare IT companies that offer software solutions and outsourcing options tailored to healthcare providers’ needs.
How do revenue cycle management services improve cash flow?
By streamlining billing processes, reducing errors, and accelerating claim submissions and payments, RCM services help healthcare providers receive payments faster and reduce the time between service delivery and revenue collection.
Are revenue cycle management services compliant with healthcare regulations?
Yes, reputable RCM service providers ensure compliance with healthcare regulations such as HIPAA (Health Insurance Portability and Accountability Act) and adhere to industry standards for data security and patient privacy.
Can revenue cycle management services be customized for different healthcare specialties?
Yes, RCM services can be tailored to meet the specific needs of various healthcare specialties, including hospitals, physician practices, dental offices, and outpatient clinics, to address unique billing and coding requirements.
What technology is used in revenue cycle management services?
RCM services often utilize advanced software platforms that integrate electronic health records (EHR), billing systems, coding tools, and analytics to automate and optimize the revenue cycle process.
How do revenue cycle management services handle denied or rejected claims?
RCM services include denial management processes that identify the reasons for claim denials, correct errors, resubmit claims, and follow up with payers to maximize reimbursement.
What are the benefits of outsourcing revenue cycle management services?
Outsourcing RCM can reduce administrative costs, improve billing accuracy, increase revenue collection, provide access to specialized expertise, and allow healthcare providers to focus more on patient care rather than financial management.







Leave a Reply