Medical billing is a complex process that serves as the bridge between healthcare providers and insurance companies. It involves translating healthcare services rendered into standardized codes that can be submitted for reimbursement. At its core, medical billing encompasses several key components, including patient registration, insurance verification, coding, claims submission, payment posting, and accounts receivable management.
Each of these elements plays a crucial role in ensuring that healthcare providers receive timely and accurate payments for their services. The intricacies of medical billing are often underestimated. It requires a deep understanding of various coding systems, such as the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT).
These codes not only facilitate the billing process but also ensure compliance with regulatory standards. Moreover, medical billing professionals must stay abreast of changes in healthcare laws and insurance policies to avoid costly errors that could lead to claim denials or delays in payment. Thus, a solid foundation in the basics of medical billing is essential for any healthcare organization aiming to maintain financial health.
Key Takeaways
- Mastering medical billing fundamentals is essential for accurate and timely reimbursement.
- Efficient coding, documentation, and claims submission streamline the billing process and reduce errors.
- Leveraging technology and data analytics enhances billing efficiency and maximizes revenue.
- Continuous staff training and patient communication improve billing accuracy and satisfaction.
- Staying compliant with regulations and effectively managing denied claims prevent revenue loss.
Implementing Efficient Coding and Documentation
Efficient coding and documentation are pivotal in the medical billing process. Accurate coding ensures that healthcare providers are reimbursed appropriately for the services they deliver. This requires meticulous attention to detail and a thorough understanding of the coding guidelines.
Medical coders must be adept at translating clinical documentation into the correct codes, which can significantly impact the revenue cycle. Inaccurate coding can lead to underpayment or overpayment, both of which can have detrimental effects on a practice’s financial stability. Documentation plays an equally important role in this process.
Comprehensive and precise documentation supports the codes assigned and serves as a defense against audits and claim denials. Healthcare providers must ensure that their clinical notes are detailed enough to justify the services billed. This not only aids in securing reimbursement but also enhances patient care by providing a clear record of treatment.
By fostering a culture of thorough documentation and efficient coding practices, healthcare organizations can streamline their billing processes and reduce the risk of revenue loss.
Streamlining the Claims Submission Process
The claims submission process is a critical juncture in medical billing that can significantly influence cash flow. Streamlining this process involves several strategies aimed at reducing errors and expediting submissions. One effective approach is to implement a standardized workflow that includes checks at each stage of the claims process.
This ensures that claims are complete and accurate before they are submitted to payers, minimizing the likelihood of denials. Additionally, adopting electronic claims submission can greatly enhance efficiency. Electronic submissions are typically processed faster than paper claims, allowing for quicker reimbursements.
By focusing on streamlining the claims submission process, healthcare organizations can improve their revenue cycle management and enhance overall financial performance.
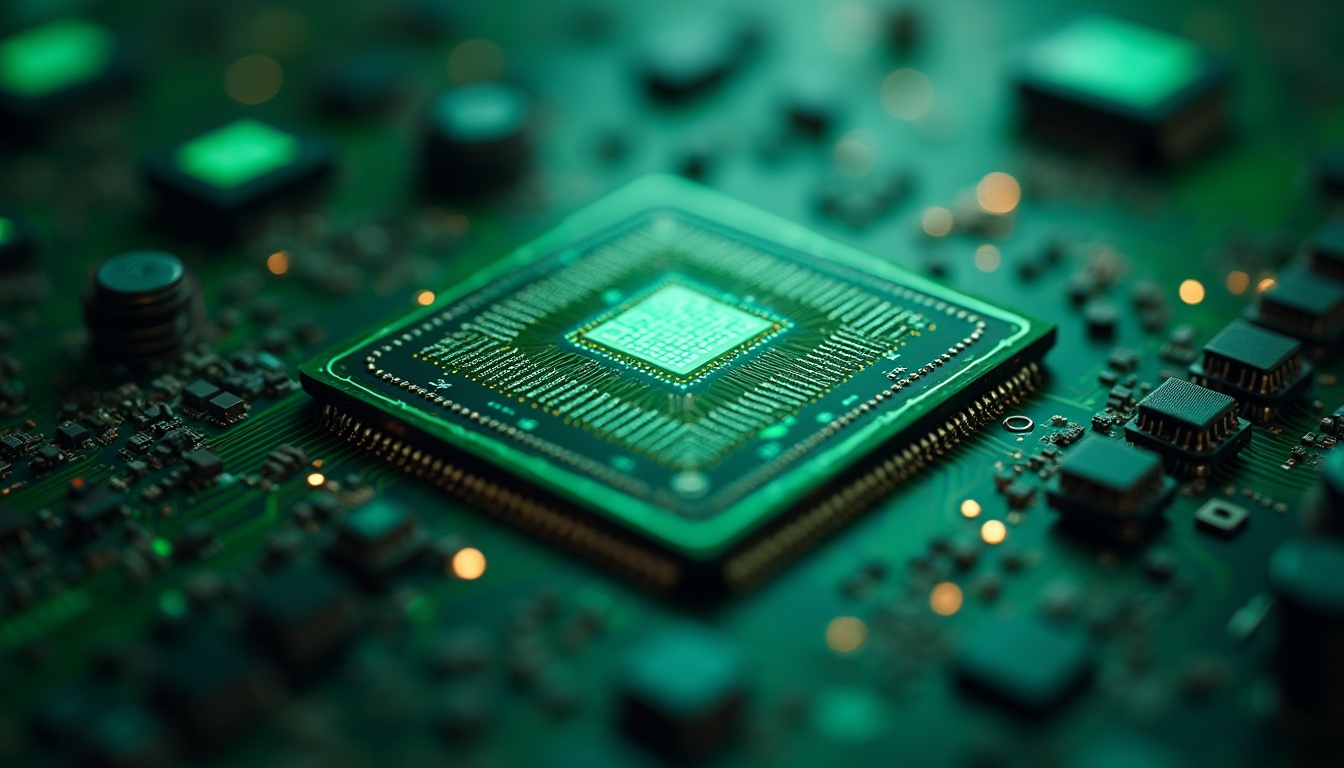
Leveraging Technology for Billing Efficiency
| Metric | Description | Before Technology Implementation | After Technology Implementation | Improvement (%) |
|---|---|---|---|---|
| Billing Cycle Time | Average time taken to generate and send invoices | 10 days | 3 days | 70% |
| Invoice Accuracy Rate | Percentage of invoices generated without errors | 85% | 98% | 15.3% |
| Payment Collection Time | Average time to receive payment after invoice issuance | 30 days | 15 days | 50% |
| Manual Data Entry Reduction | Reduction in manual input required for billing | 100% | 20% | 80% |
| Cost per Invoice | Average operational cost to process one invoice | 5 units | 2 units | 60% |
| Customer Dispute Rate | Percentage of invoices disputed by customers | 12% | 4% | 66.7% |
In today’s digital age, leveraging technology is essential for achieving billing efficiency in healthcare organizations. Advanced billing software solutions can automate many aspects of the billing process, from patient registration to claims submission and payment tracking. These systems not only reduce manual errors but also save time by streamlining workflows and improving data accuracy.
Moreover, technology can facilitate better communication between healthcare providers and payers. For instance, real-time eligibility verification tools allow providers to confirm a patient’s insurance coverage before services are rendered, reducing the chances of claim denials due to coverage issues. Additionally, analytics tools can provide insights into billing trends and performance metrics, enabling organizations to identify areas for improvement.
By embracing technology, healthcare organizations can enhance their billing processes and ultimately improve their financial outcomes.
Optimizing the Revenue Cycle Management
Optimizing revenue cycle management (RCM) is crucial for ensuring that healthcare organizations maintain financial viability. RCM encompasses all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue. To optimize RCM, organizations must adopt a holistic approach that addresses each stage of the revenue cycle.
One effective strategy is to conduct regular audits of billing practices to identify inefficiencies and areas for improvement. This may involve analyzing key performance indicators (KPIs) such as days in accounts receivable, claim denial rates, and collection rates. By understanding these metrics, organizations can implement targeted interventions to enhance their RCM processes.
Additionally, fostering collaboration between clinical and administrative teams can lead to improved communication and more efficient workflows, ultimately resulting in better financial performance.
Improving Patient Communication and Education on Billing
Effective patient communication is an often-overlooked aspect of medical billing that can significantly impact revenue collection. Patients who understand their financial responsibilities are more likely to pay their bills on time, reducing accounts receivable days for healthcare providers. Therefore, it is essential for organizations to prioritize patient education regarding billing processes and insurance coverage.
Providing clear and concise information about costs upfront can help set realistic expectations for patients. This may include offering estimates for services based on insurance coverage or providing detailed explanations of out-of-pocket expenses. Additionally, organizations should establish open lines of communication for patients to ask questions about their bills or payment options.
By fostering a culture of transparency and support, healthcare providers can enhance patient satisfaction while improving their overall revenue cycle.
Training Staff for Effective Billing Practices
Staff training is a critical component of effective medical billing practices. A well-trained team is essential for navigating the complexities of coding, documentation, and claims submission. Regular training sessions can help staff stay updated on changes in regulations, coding guidelines, and billing software functionalities.
Moreover, investing in ongoing education fosters a culture of continuous improvement within the organization. Staff members who feel confident in their skills are more likely to produce accurate work and contribute positively to the revenue cycle. Training should also emphasize the importance of collaboration between clinical and administrative teams to ensure seamless communication throughout the billing process.
By prioritizing staff training, healthcare organizations can enhance their billing efficiency and reduce the risk of costly errors.
Utilizing Data Analytics for Revenue Maximization
Data analytics has emerged as a powerful tool for maximizing revenue in healthcare organizations. By harnessing data from various sources, organizations can gain valuable insights into their billing processes and identify trends that may impact revenue generation. For instance, analyzing claim denial patterns can help pinpoint common issues that lead to rejected claims, allowing organizations to address these problems proactively.
Furthermore, predictive analytics can assist in forecasting future revenue based on historical data trends. This enables organizations to make informed decisions regarding resource allocation and strategic planning. By leveraging data analytics effectively, healthcare providers can optimize their revenue cycle management efforts and enhance overall financial performance.
Addressing Denied Claims and Revenue Leakage
Denied claims represent a significant source of revenue leakage for healthcare organizations. Addressing this issue requires a systematic approach to identifying the root causes of denials and implementing corrective measures. Organizations should establish a dedicated team responsible for tracking denied claims and analyzing denial trends to uncover underlying issues.
Once patterns are identified, targeted interventions can be implemented to reduce future denials. This may involve revising coding practices, improving documentation standards, or enhancing staff training on payer requirements. Additionally, maintaining open communication with payers can facilitate quicker resolutions for denied claims.
By proactively addressing denied claims and minimizing revenue leakage, healthcare organizations can significantly improve their financial health.
Outsourcing Medical Billing Services for Efficiency
Outsourcing medical billing services has become an increasingly popular option for healthcare organizations seeking efficiency and cost savings. By partnering with specialized billing companies, providers can leverage expertise in coding, compliance, and revenue cycle management without the overhead costs associated with maintaining an in-house billing team. Outsourcing allows healthcare organizations to focus on their core competencies—delivering quality patient care—while leaving the complexities of billing to experts in the field.
Additionally, outsourced billing services often utilize advanced technology solutions that enhance efficiency and accuracy in the billing process. This partnership can lead to improved cash flow and reduced administrative burdens for healthcare providers.
Staying Updated on Billing Regulations and Compliance
The landscape of medical billing is constantly evolving due to changes in regulations and compliance requirements. Staying updated on these changes is essential for healthcare organizations to avoid costly penalties and ensure proper reimbursement for services rendered. Regular training sessions focused on regulatory updates should be implemented as part of staff development programs.
Moreover, subscribing to industry newsletters or joining professional associations can provide valuable insights into emerging trends and best practices in medical billing.
In conclusion, navigating the complexities of medical billing requires a multifaceted approach that encompasses efficient coding practices, streamlined processes, effective communication with patients, staff training, data analytics utilization, proactive denial management, outsourcing options, and staying informed about regulatory changes.
By implementing these strategies holistically, healthcare organizations can optimize their revenue cycle management efforts while ensuring financial stability in an ever-evolving industry landscape.
In the realm of revenue cycle medical billing, understanding the impact of automation can significantly enhance efficiency and accuracy. A related article that delves into this topic is titled “AI Coach Assist: An Automated Approach for Call Management,” which discusses how AI can streamline communication processes within the billing cycle. You can read more about it by following this link: AI Coach Assist: An Automated Approach for Call Management.
FAQs
What is revenue cycle medical billing?
Revenue cycle medical billing is the process healthcare providers use to manage the financial transactions related to patient services. It involves submitting and following up on claims with health insurance companies to receive payment for services rendered.
Why is revenue cycle management important in healthcare?
Revenue cycle management is crucial because it ensures that healthcare providers are properly reimbursed for their services. Efficient management helps maintain cash flow, reduces errors, and improves overall financial performance.
What are the main steps involved in the revenue cycle medical billing process?
The main steps include patient registration, insurance verification, charge capture, claim submission, payment posting, denial management, and patient billing.
Who is responsible for revenue cycle medical billing?
Typically, medical billing specialists or revenue cycle management teams within healthcare organizations handle the billing process. Some providers outsource this function to specialized billing companies.
What is the difference between medical coding and medical billing?
Medical coding involves translating healthcare services into standardized codes, while medical billing uses those codes to create and submit claims to insurance companies for payment.
How do insurance claims work in revenue cycle medical billing?
After services are provided, claims are submitted to insurance companies detailing the procedures performed. The insurer reviews the claim, processes payment based on coverage, and sends an explanation of benefits to both the provider and patient.
What are common challenges in revenue cycle medical billing?
Challenges include claim denials, coding errors, delayed payments, insurance verification issues, and maintaining compliance with changing regulations.
How can healthcare providers improve their revenue cycle management?
Providers can improve by implementing efficient billing software, training staff, verifying insurance eligibility upfront, promptly addressing denials, and regularly auditing billing processes.
What role does technology play in revenue cycle medical billing?
Technology automates many billing tasks, reduces errors, speeds up claim processing, and provides analytics to optimize revenue cycle performance.
What is denial management in medical billing?
Denial management involves identifying, analyzing, and resolving rejected or denied insurance claims to ensure proper reimbursement for services provided.








Leave a Reply