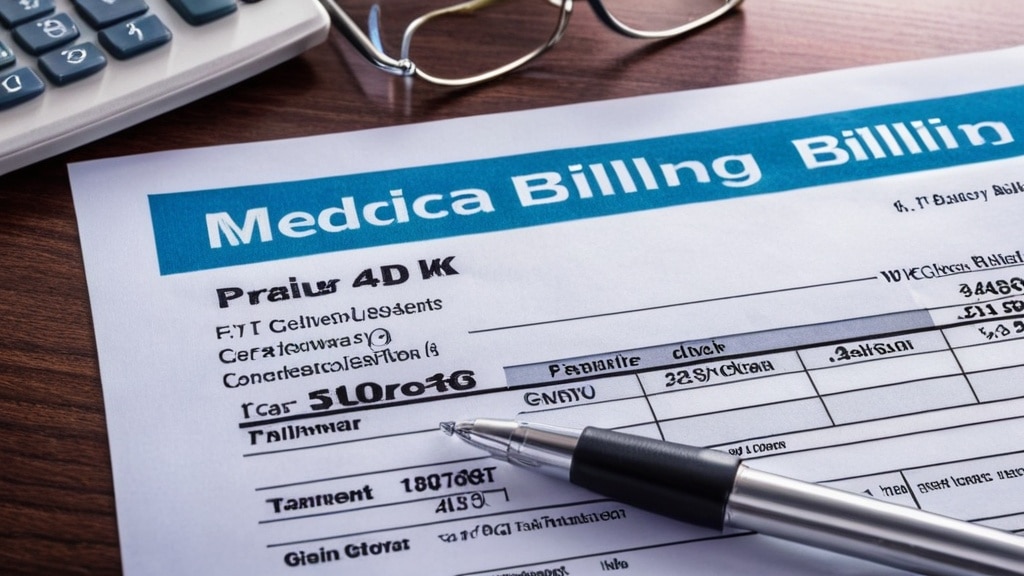
Effective medical billing is a cornerstone of the healthcare industry, serving as the bridge between patient care and financial sustainability. It is not merely a back-office function; rather, it plays a pivotal role in ensuring that healthcare providers receive timely and accurate compensation for the services they deliver. The intricacies of medical billing encompass a wide range of activities, from coding diagnoses and procedures to submitting claims and managing denials.
When executed efficiently, medical billing can significantly enhance a healthcare organization’s cash flow, allowing it to reinvest in patient care and improve overall service delivery. Moreover, effective medical billing is essential for maintaining compliance with various regulations and standards. The healthcare landscape is fraught with complexities, including ever-evolving policies and payer requirements.
A robust billing process not only safeguards against financial losses but also mitigates the risk of audits and penalties that can arise from non-compliance. In this context, understanding the importance of effective medical billing transcends financial implications; it is integral to the operational health of any healthcare organization.
Key Takeaways
- Effective medical billing is crucial for optimizing healthcare revenue and ensuring smooth financial operations.
- Accurate coding, documentation, and timely claim submissions reduce denials and improve reimbursement rates.
- Leveraging technology and outsourcing billing services can enhance efficiency and streamline billing workflows.
- Continuous staff training and staying informed on healthcare policy changes ensure compliance and best practices.
- Clear patient communication about billing fosters transparency and reduces payment delays.
Implementing Efficient Coding and Documentation
The foundation of effective medical billing lies in accurate coding and thorough documentation. Coding involves translating medical diagnoses, procedures, and services into universally recognized alphanumeric codes, which are then used for billing purposes. Efficient coding is crucial because it directly impacts reimbursement rates and the likelihood of claim approval.
Inaccurate or incomplete coding can lead to claim denials, delayed payments, and ultimately, revenue loss. Therefore, healthcare organizations must prioritize training their coding staff to ensure they are well-versed in the latest coding systems, such as ICD-10 and CPT. Documentation plays an equally vital role in the billing process.
Comprehensive documentation not only supports the codes assigned but also provides a clear narrative of the patient’s care journey. This narrative is essential for justifying claims to payers and defending against potential audits. Implementing standardized documentation practices can streamline this process, ensuring that all necessary information is captured consistently.
By fostering a culture of meticulous documentation and efficient coding, healthcare organizations can significantly reduce errors and enhance their overall billing efficiency.
Utilizing Technology for Streamlined Billing Processes

In today’s digital age, leveraging technology is imperative for streamlining medical billing processes. Advanced billing software solutions can automate many aspects of the billing cycle, from appointment scheduling to claim submission. These systems can reduce manual errors, enhance data accuracy, and expedite the billing process, ultimately leading to faster reimbursements.
Additionally, technology can facilitate real-time tracking of claims, allowing organizations to monitor their status and address any issues promptly. Moreover, integrating electronic health records (EHR) with billing systems can create a seamless flow of information between clinical and administrative functions. This integration ensures that patient data is readily available for coding and billing purposes, reducing the likelihood of discrepancies.
By harnessing technology effectively, healthcare organizations can not only improve their operational efficiency but also enhance the patient experience by minimizing billing-related delays and confusion.
Ensuring Accurate and Timely Submission of Claims
| Metric | Description | Target | Current Value | Frequency Measured |
|---|---|---|---|---|
| Claim Submission Accuracy Rate | Percentage of claims submitted without errors | 98% | 95% | Monthly |
| Average Time to Submit Claims | Average number of days from service date to claim submission | 2 days | 3 days | Monthly |
| Claims Rejection Rate | Percentage of claims rejected due to errors or missing information | Less than 2% | 4% | Monthly |
| Claims Resubmission Rate | Percentage of claims that require resubmission after initial rejection | Less than 3% | 5% | Monthly |
| On-Time Submission Rate | Percentage of claims submitted within the required timeframe | 99% | 97% | Monthly |
| Staff Training Completion Rate | Percentage of claims processing staff trained on submission protocols | 100% | 90% | Quarterly |
The submission of claims is a critical juncture in the medical billing process that requires precision and timeliness. Accurate claims submission is essential for ensuring that healthcare providers receive appropriate reimbursement for their services. Errors in claims can lead to denials or delays in payment, which can have cascading effects on an organization’s cash flow.
Therefore, it is vital for billing teams to implement rigorous checks and balances to verify the accuracy of claims before submission. Timeliness is equally important; many payers have strict deadlines for claim submissions. Delayed submissions can result in lost revenue opportunities or reduced reimbursement rates.
To combat this challenge, healthcare organizations should establish clear workflows that prioritize timely claim submissions while maintaining accuracy. Regular audits of submitted claims can also help identify patterns of errors or delays, enabling organizations to refine their processes continually.
Minimizing Denials and Rejections through Proper Billing Practices
Denials and rejections are significant pain points in the medical billing process that can lead to substantial revenue loss. Understanding the common reasons behind these denials is crucial for developing effective strategies to minimize them. Common causes include incorrect patient information, lack of medical necessity documentation, or coding errors.
By addressing these issues proactively, healthcare organizations can significantly reduce the frequency of denials. Implementing best practices in billing can also play a pivotal role in minimizing rejections. This includes conducting thorough eligibility checks before services are rendered, ensuring that all necessary documentation is collected upfront, and maintaining open lines of communication with payers.
Additionally, establishing a dedicated team to manage denials can help organizations analyze trends and develop targeted interventions to address recurring issues. By fostering a proactive approach to billing practices, healthcare organizations can enhance their revenue cycle management and improve overall financial health.
Maximizing Reimbursements with Strategic Negotiations

Maximizing reimbursements requires more than just accurate coding and timely submissions; it often involves strategic negotiations with payers as well. Understanding the nuances of payer contracts and reimbursement rates is essential for healthcare organizations seeking to optimize their revenue streams. Engaging in negotiations with payers can lead to more favorable terms that enhance reimbursement rates for services rendered.
To effectively negotiate with payers, healthcare organizations must be armed with data-driven insights regarding their service utilization patterns and market benchmarks. This information can provide leverage during negotiations, allowing organizations to advocate for fair compensation based on their unique value proposition. Additionally, fostering strong relationships with payer representatives can facilitate smoother negotiations and open doors for future collaborations.
By adopting a strategic approach to negotiations, healthcare organizations can significantly enhance their financial outcomes.
Improving Patient Communication and Education on Billing Matters
Effective communication with patients regarding billing matters is essential for fostering trust and transparency in the healthcare experience. Patients often encounter confusion surrounding their bills due to complex terminology or unexpected charges. By proactively educating patients about their financial responsibilities and the billing process, healthcare organizations can alleviate anxiety and improve satisfaction levels.
Implementing clear communication strategies—such as providing detailed explanations of charges upfront or offering financial counseling services—can empower patients to make informed decisions about their care. Additionally, utilizing digital platforms to share billing information can enhance accessibility and convenience for patients. By prioritizing patient education on billing matters, healthcare organizations can not only improve patient satisfaction but also reduce the likelihood of payment delays or disputes.
Monitoring and Analyzing Key Performance Indicators for Revenue Optimization
To optimize revenue effectively, healthcare organizations must establish a framework for monitoring and analyzing key performance indicators (KPIs) related to their billing processes. KPIs such as days in accounts receivable, claim denial rates, and collection rates provide valuable insights into the efficiency of the revenue cycle management process. Regularly reviewing these metrics allows organizations to identify areas for improvement and implement targeted interventions.
Moreover, benchmarking KPIs against industry standards can provide context for performance evaluation. Understanding how an organization compares to peers can highlight strengths and weaknesses within its billing practices. By fostering a culture of continuous improvement through data analysis, healthcare organizations can enhance their revenue optimization efforts and ensure long-term financial sustainability.
Training and Educating Staff on Best Billing Practices
The success of any medical billing operation hinges on the expertise of its staff. Therefore, investing in training and education is paramount for ensuring that billing teams are equipped with the knowledge and skills necessary to navigate the complexities of medical billing effectively. Regular training sessions on coding updates, regulatory changes, and best practices can empower staff to perform their roles with confidence.
Additionally, fostering a culture of collaboration among billing staff can enhance knowledge sharing and problem-solving capabilities.
By prioritizing staff training and education on best practices, healthcare organizations can cultivate a highly skilled workforce that drives efficiency and accuracy in medical billing.
Outsourcing Billing Services for Increased Efficiency and Revenue
Outsourcing medical billing services has emerged as a viable strategy for many healthcare organizations seeking increased efficiency and revenue optimization. Partnering with specialized billing companies allows organizations to leverage expertise in revenue cycle management while freeing up internal resources to focus on core clinical functions. Outsourcing can lead to improved accuracy in coding, faster claim submissions, and reduced administrative burdens.
Moreover, outsourcing partners often employ advanced technology solutions that enhance data analytics capabilities and streamline processes further. This collaboration can result in higher collection rates and reduced denial rates due to the specialized knowledge that external partners bring to the table. By considering outsourcing as part of their overall strategy, healthcare organizations can achieve greater operational efficiency while maximizing revenue potential.
Staying Updated on Changes in Healthcare Policies and Regulations for Billing Compliance
The healthcare landscape is constantly evolving, with new policies and regulations emerging regularly that impact medical billing practices. Staying updated on these changes is crucial for ensuring compliance and avoiding potential penalties or audits. Healthcare organizations must establish mechanisms for monitoring regulatory updates from relevant authorities such as Medicare, Medicaid, and private payers.
Regular training sessions focused on compliance updates should be integrated into staff education programs to ensure that all team members are aware of current regulations affecting billing practices. Additionally, designating compliance officers or teams responsible for overseeing adherence to regulations can further strengthen an organization’s commitment to compliance. By prioritizing awareness of changes in healthcare policies and regulations, healthcare organizations can safeguard against compliance risks while enhancing their overall billing practices.
In conclusion, effective medical billing is an intricate process that requires a multifaceted approach encompassing efficient coding practices, technology utilization, timely submissions, strategic negotiations, patient communication, performance monitoring, staff training, outsourcing considerations, and regulatory compliance awareness. By addressing each aspect diligently, healthcare organizations can optimize their revenue cycle management efforts while ensuring financial sustainability in an increasingly complex healthcare environment.
Effective revenue cycle management is crucial for optimizing medical billing processes and ensuring financial stability in healthcare organizations. For insights on how artificial intelligence can enhance team performance in this area, you may find the article on ai/2025/09/15/leveraging-ai-coaching-to-unlock-your-teams-full-potential/’>leveraging AI coaching to unlock your team’s full potential particularly informative.
This resource discusses innovative strategies that can help streamline operations and improve overall efficiency in revenue cycle management.
FAQs
What is revenue cycle management in medical billing?
Revenue cycle management (RCM) in medical billing refers to the process of managing the financial transactions and administrative functions associated with patient services, from scheduling appointments to final payment collection. It ensures healthcare providers are properly reimbursed for their services.
Why is revenue cycle management important for healthcare providers?
RCM is important because it helps healthcare providers maintain financial stability by streamlining billing processes, reducing claim denials, improving cash flow, and ensuring timely payments from insurance companies and patients.
What are the key steps involved in revenue cycle management?
The key steps include patient registration, insurance verification, charge capture, claim submission, payment posting, denial management, and patient billing and collections.
How does insurance verification impact revenue cycle management?
Insurance verification confirms a patient’s coverage and benefits before services are rendered, reducing claim denials and delays in payment, which improves the overall efficiency of the revenue cycle.
What role does technology play in revenue cycle management?
Technology, such as electronic health records (EHR) and billing software, automates many RCM tasks, improves accuracy, speeds up claim processing, and provides real-time analytics to optimize revenue collection.
What are common challenges in revenue cycle management?
Common challenges include claim denials, coding errors, delayed payments, complex insurance policies, and maintaining compliance with healthcare regulations.
How can healthcare providers improve their revenue cycle management?
Providers can improve RCM by investing in staff training, using advanced billing software, regularly auditing billing processes, verifying insurance information accurately, and promptly addressing claim denials.
What is the difference between medical billing and revenue cycle management?
Medical billing is a component of revenue cycle management focused specifically on submitting and following up on claims with health insurance companies. RCM encompasses the entire financial process from patient intake to final payment.
Who is responsible for revenue cycle management in a healthcare organization?
Typically, a dedicated RCM team or department handles these tasks, which may include billing specialists, coders, patient financial counselors, and revenue cycle managers.
Can outsourcing revenue cycle management benefit medical practices?
Yes, outsourcing RCM can help medical practices reduce administrative burdens, improve billing accuracy, increase collections, and allow providers to focus more on patient care.








Leave a Reply