Revenue Cycle Management (RCM) billing is a critical process that encompasses the entire financial journey of a healthcare service, from patient registration to the final payment. It involves a series of steps that ensure healthcare providers receive timely and accurate reimbursement for their services. Understanding RCM billing is essential for healthcare organizations aiming to optimize their financial performance and enhance patient satisfaction.
The complexity of RCM billing arises from the multitude of regulations, payer requirements, and the intricacies of healthcare services, making it imperative for practices to have a robust system in place.
This includes verifying insurance eligibility, coding services accurately, submitting claims, and following up on payments.
Each step in the RCM process is interconnected, and inefficiencies at any point can lead to delayed payments or revenue loss. As healthcare continues to evolve with new technologies and regulations, understanding the nuances of RCM billing becomes increasingly important for providers who wish to maintain financial health and compliance.
Key Takeaways
- RCM billing integrates multiple components to optimize healthcare revenue cycles.
- Selecting and implementing the right RCM system is crucial for practice efficiency.
- Accurate coding, documentation, and error reduction improve billing success.
- Analytics and reporting help identify revenue opportunities and streamline processes.
- Staff training and deciding between outsourcing or in-house billing impact overall RCM effectiveness.
Key Components of RCM Billing
The key components of RCM billing include patient registration, charge capture, claim submission, payment posting, and accounts receivable management. Each of these elements plays a vital role in ensuring that healthcare providers are compensated for their services. Patient registration is the first step in the process, where essential information such as demographics and insurance details are collected.
Accurate data at this stage is crucial, as it sets the foundation for the entire billing cycle. Charge capture involves documenting the services provided to patients and translating them into billable codes. This step requires meticulous attention to detail, as errors in coding can lead to claim denials or underpayments.
Once charges are captured, claims are submitted to insurance companies for reimbursement. The claim submission process must adhere to specific payer guidelines to ensure timely processing. After claims are submitted, payment posting occurs, where payments from insurers and patients are recorded.
Finally, accounts receivable management involves tracking outstanding payments and following up on any unpaid claims, ensuring that revenue flows smoothly into the practice.
Choosing the Right RCM Billing System

Selecting the right RCM billing system is a pivotal decision for any healthcare organization. The ideal system should align with the specific needs of the practice while offering features that enhance efficiency and accuracy. When evaluating RCM billing systems, it is essential to consider factors such as ease of use, integration capabilities with existing electronic health record (EHR) systems, and compliance with industry regulations.
A user-friendly interface can significantly reduce training time for staff and improve overall productivity. Moreover, scalability is another critical aspect to consider when choosing an RCM billing system. As practices grow or change, their billing needs may evolve as well.
A flexible system that can adapt to these changes will provide long-term value. Additionally, it is important to assess the level of customer support offered by the vendor. Reliable support can make a significant difference in resolving issues quickly and minimizing disruptions in the billing process.
Implementing RCM Billing in Your Practice
| Metric | Description | Typical Value/Range | Impact on Practice |
|---|---|---|---|
| Claim Submission Rate | Percentage of claims submitted accurately on first attempt | 85% – 95% | Higher rates reduce delays and improve cash flow |
| Claim Denial Rate | Percentage of claims denied by payers | 5% – 15% | Lower denial rates increase revenue and reduce administrative burden |
| Days in Accounts Receivable (A/R) | Average number of days to collect payment after service | 30 – 45 days | Shorter A/R cycles improve cash flow and financial stability |
| Clean Claim Rate | Percentage of claims processed without errors | 90% – 98% | High clean claim rates reduce rework and speed up payments |
| Patient Payment Collection Rate | Percentage of patient balances collected at point of service or billing | 70% – 90% | Improves overall revenue and reduces bad debt |
| Cost to Collect | Average cost incurred to collect each unit of revenue | Variable, typically 3% – 7% of revenue | Lower costs increase net revenue and profitability |
| Revenue Cycle Turnaround Time | Time from patient registration to final payment | 20 – 40 days | Faster turnaround improves cash flow and operational efficiency |
Implementing an RCM billing system in your practice requires careful planning and execution. The first step is to conduct a thorough assessment of your current billing processes to identify areas for improvement. This assessment should involve input from key stakeholders, including administrative staff, billing personnel, and clinical teams.
By understanding the existing workflow and pinpointing inefficiencies, practices can tailor their implementation strategy to address specific challenges. Once the assessment is complete, it is essential to develop a comprehensive implementation plan that outlines timelines, responsibilities, and training requirements. Engaging staff early in the process can foster buy-in and facilitate a smoother transition.
Training sessions should be conducted to familiarize employees with the new system and its functionalities. Ongoing support during the implementation phase is crucial to address any questions or concerns that may arise as staff adapt to the new processes.
Maximizing Revenue with RCM Billing
Maximizing revenue through effective RCM billing involves a proactive approach to managing the entire revenue cycle. One key strategy is to ensure accurate coding and documentation from the outset. By capturing all billable services accurately, practices can avoid revenue leakage due to undercoding or missed charges.
Regular audits of coding practices can help identify trends and areas for improvement. Additionally, timely follow-up on outstanding claims is essential for maintaining cash flow. Establishing a systematic approach to accounts receivable management can help practices identify delinquent accounts early and take appropriate action.
This may involve sending reminders to patients or working with payers to resolve any issues with claims processing. By actively managing the revenue cycle, practices can enhance their financial performance and reduce the risk of cash flow disruptions.
Streamlining the Billing Process

Streamlining the billing process is vital for improving efficiency and reducing administrative burdens on staff. One effective way to achieve this is by automating repetitive tasks within the RCM workflow. Automation tools can assist with tasks such as claim submission, payment posting, and follow-up reminders, allowing staff to focus on more complex issues that require human intervention.
Another approach to streamlining billing is to standardize processes across the organization. Developing clear protocols for each step in the revenue cycle can help ensure consistency and reduce errors. Regular training sessions can reinforce these protocols and keep staff updated on any changes in regulations or payer requirements.
By fostering a culture of continuous improvement, practices can enhance their billing processes over time.
Coding and Documentation Best Practices
Adhering to coding and documentation best practices is essential for ensuring compliance and maximizing reimbursement in RCM billing. Accurate coding not only affects revenue but also impacts patient care quality and outcomes. Healthcare providers should stay informed about current coding guidelines and updates from organizations such as the American Medical Association (AMA) and the Centers for Medicare & Medicaid Services (CMS).
Documentation plays a crucial role in supporting coding decisions. Providers must ensure that clinical documentation accurately reflects the services rendered and justifies the codes used for billing purposes. Regular training on documentation standards can help clinicians understand what information is necessary for compliance and reimbursement.
Additionally, implementing a peer review process can provide an extra layer of oversight to catch potential errors before claims are submitted.
Reducing Billing Errors and Denials
Reducing billing errors and denials is a critical goal for any healthcare organization seeking to optimize its revenue cycle management efforts. Common causes of denials include incorrect patient information, coding errors, and lack of medical necessity documentation. To mitigate these issues, practices should implement thorough verification processes at each stage of the revenue cycle.
One effective strategy is to conduct regular audits of denied claims to identify patterns and root causes of errors. By analyzing denial trends, practices can develop targeted interventions to address specific issues. Additionally, fostering open communication between clinical staff and billing personnel can help ensure that all necessary information is captured accurately during patient encounters.
By prioritizing accuracy and collaboration, practices can significantly reduce billing errors and improve overall revenue performance.
Leveraging Analytics and Reporting for Revenue Optimization
Analytics and reporting play a crucial role in optimizing revenue cycle management by providing insights into financial performance and operational efficiency. By leveraging data analytics tools, healthcare organizations can track key performance indicators (KPIs) such as days in accounts receivable, claim denial rates, and collection rates. These metrics offer valuable insights into areas that require attention or improvement.
Regular reporting allows practices to monitor trends over time and make data-driven decisions regarding their revenue cycle strategies. For instance, if a particular payer consistently shows high denial rates, practices can investigate further to understand the underlying issues and adjust their approach accordingly. By utilizing analytics effectively, organizations can enhance their revenue optimization efforts and drive continuous improvement within their RCM processes.
Training Staff for RCM Billing Success
Training staff effectively is paramount for achieving success in revenue cycle management billing. A well-trained team is better equipped to navigate complex billing processes, adhere to compliance standards, and minimize errors. Training programs should be comprehensive and tailored to meet the specific needs of different roles within the organization.
Regular workshops or refresher courses can reinforce best practices and encourage continuous learning among employees. By investing in staff training, healthcare organizations can foster a culture of excellence in revenue cycle management that ultimately leads to improved financial outcomes.
Outsourcing RCM Billing vs In-house Management
When considering revenue cycle management options, healthcare organizations often face the decision between outsourcing RCM billing or managing it in-house. Each approach has its advantages and disadvantages that must be carefully weighed based on the specific needs of the practice. Outsourcing RCM billing can provide access to specialized expertise and advanced technology without requiring significant upfront investment in infrastructure or personnel training.
Third-party vendors often have established processes in place that can lead to improved efficiency and reduced errors. However, outsourcing may also result in less control over the billing process and potential communication challenges between external vendors and internal staff. On the other hand, managing RCM billing in-house allows for greater control over processes and direct oversight of staff performance.
This approach may foster stronger relationships between clinical teams and billing personnel, leading to improved collaboration on documentation and coding practices. However, it also requires ongoing investment in training and technology updates to remain competitive in an evolving healthcare landscape. Ultimately, the decision between outsourcing or in-house management should be based on a thorough assessment of organizational goals, resources available, and long-term strategic plans for revenue cycle management success.
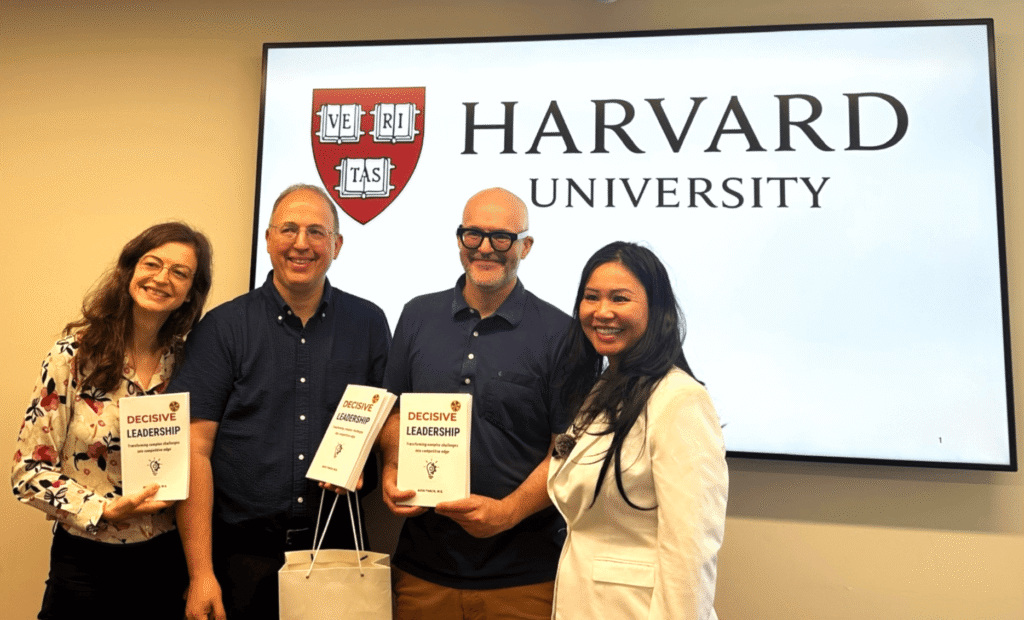
In the realm of revenue cycle management (RCM) billing, understanding the impact of leadership and decision-making in AI can be crucial for optimizing processes. A related article that delves into this topic is titled “Leadership in AI: Executive Decision Making,” which explores how effective leadership can drive AI initiatives within organizations. You can read more about it [here](https://iavva.ai/business/leadership-in-ai-executive-decision-making/). This insight can be particularly beneficial for RCM professionals looking to leverage AI technologies to enhance billing efficiency and accuracy.
FAQs
What is RCM billing?
RCM billing stands for Revenue Cycle Management billing. It is the process used by healthcare providers to track patient care episodes from registration and appointment scheduling to the final payment of a balance. The goal is to optimize the financial performance of healthcare organizations by managing claims, payments, and revenue generation efficiently.
Why is RCM billing important in healthcare?
RCM billing is crucial because it ensures that healthcare providers are properly reimbursed for their services. Efficient RCM processes reduce claim denials, speed up payment cycles, and improve cash flow, which ultimately supports the sustainability and growth of healthcare practices.
What are the key components of RCM billing?
The key components of RCM billing include patient registration, insurance verification, charge capture, claim submission, payment posting, denial management, and patient collections. Each step is essential to ensure accurate billing and timely reimbursement.
Who is responsible for RCM billing?
RCM billing is typically managed by a dedicated billing department within a healthcare organization or outsourced to specialized RCM service providers. Medical coders, billers, and revenue cycle analysts work together to handle the various stages of the billing process.
How does RCM billing affect patient experience?
Effective RCM billing can improve patient experience by providing clear communication about billing and payment options, reducing billing errors, and offering flexible payment plans. This transparency helps build trust between patients and healthcare providers.
What challenges are associated with RCM billing?
Challenges in RCM billing include dealing with complex insurance policies, claim denials, regulatory compliance, data accuracy, and maintaining up-to-date technology. These challenges require continuous monitoring and process improvement to minimize revenue loss.
Can technology improve RCM billing?
Yes, technology such as electronic health records (EHR), billing software, and automated claim processing systems can significantly improve the efficiency and accuracy of RCM billing. These tools help reduce manual errors, speed up claim submissions, and provide real-time analytics for better decision-making.
What is the difference between RCM billing and medical billing?
Medical billing is a component of the broader RCM process. While medical billing focuses specifically on submitting and following up on claims with health insurance companies, RCM encompasses the entire financial process from patient intake to final payment collection.
How can healthcare providers optimize their RCM billing process?
Providers can optimize RCM billing by implementing standardized workflows, investing in staff training, utilizing advanced billing software, regularly auditing billing practices, and staying updated with regulatory changes. Partnering with experienced RCM service providers can also enhance efficiency.
Is RCM billing regulated?
Yes, RCM billing is subject to various regulations such as HIPAA (Health Insurance Portability and Accountability Act) in the United States, which governs patient data privacy and security. Compliance with payer-specific rules and government healthcare programs is also mandatory.






Leave a Reply