Revenue Cycle Management (RCM) is a critical component of the healthcare industry, encompassing the entire process of managing claims, payment, and revenue generation. It begins with patient registration and continues through the final payment of a balance. RCM is not merely a back-office function; it is a strategic process that directly impacts the financial health of healthcare organizations.
Understanding RCM involves recognizing its multifaceted nature, which includes patient scheduling, insurance verification, coding, billing, and collections. Each step in this cycle is interconnected, and inefficiencies at any point can lead to significant revenue loss. The importance of RCM cannot be overstated, as it serves as the backbone of financial sustainability for healthcare providers.
A well-structured RCM process ensures that healthcare organizations can deliver quality care while maintaining profitability. It also plays a vital role in patient satisfaction, as timely and accurate billing contributes to a positive patient experience. As healthcare continues to evolve with new regulations and technologies, understanding the nuances of RCM becomes increasingly essential for providers aiming to thrive in a competitive landscape.
Key Takeaways
- Effective Revenue Cycle Management (RCM) is crucial for optimizing medical billing and ensuring steady cash flow.
- Leveraging technology and data analytics enhances efficiency and identifies new revenue opportunities.
- Accurate coding, documentation, and streamlined claims processing reduce errors and speed up payments.
- Engaging patients and addressing denials promptly improve timely payments and maximize revenue.
- Ongoing staff training, compliance adherence, and continuous process monitoring are key to sustained RCM success.
Implementing Best Practices for RCM in Medical Billing
To optimize Revenue Cycle Management, healthcare organizations must implement best practices that streamline processes and enhance efficiency. One of the foundational best practices is ensuring accurate patient information at the point of entry. This includes verifying insurance coverage and collecting necessary demographic details before services are rendered.
By establishing a robust front-end process, organizations can reduce claim denials and expedite payment cycles, ultimately improving cash flow. Another critical best practice involves regular training and education for staff involved in the RCM process. Continuous professional development ensures that employees are up-to-date with the latest coding guidelines, payer requirements, and regulatory changes.
This knowledge empowers staff to navigate the complexities of medical billing more effectively, reducing errors and enhancing overall performance.
Leveraging Technology for Efficient RCM

In today’s digital age, leveraging technology is paramount for achieving efficient Revenue Cycle Management. Advanced software solutions can automate various aspects of the RCM process, from patient registration to claims submission and payment posting. By utilizing electronic health records (EHR) integrated with billing systems, healthcare organizations can streamline workflows and minimize manual data entry errors.
This integration not only enhances accuracy but also accelerates the overall revenue cycle. Moreover, technology enables real-time analytics and reporting, providing organizations with valuable insights into their financial performance. By analyzing key performance indicators (KPIs), such as days in accounts receivable and claim denial rates, healthcare providers can identify areas for improvement and make data-driven decisions.
Implementing technology solutions also facilitates better communication between departments, ensuring that all stakeholders are aligned in their efforts to optimize revenue generation.
Streamlining the Claims Process for Faster Revenue Generation
| Metric | Description | Before Streamlining | After Streamlining | Improvement |
|---|---|---|---|---|
| Average Claim Processing Time | Time taken from claim submission to resolution (in days) | 15 | 7 | 53% Reduction |
| Claim Approval Rate | Percentage of claims approved on first submission | 70% | 85% | 15% Increase |
| Revenue Cycle Time | Time from claim approval to revenue collection (in days) | 20 | 10 | 50% Reduction |
| Claim Denial Rate | Percentage of claims denied due to errors or missing info | 12% | 5% | 58% Reduction |
| Cost per Claim Processed | Average operational cost to process a single claim | 30 | 18 | 40% Reduction |
| Customer Satisfaction Score | Rating from customers on claims experience (scale 1-10) | 6.5 | 8.7 | 34% Improvement |
The claims process is a pivotal element of Revenue Cycle Management that directly influences cash flow. Streamlining this process involves several strategies aimed at reducing delays and enhancing efficiency. One effective approach is to implement a centralized claims management system that allows for real-time tracking of claims status.
This visibility enables staff to identify bottlenecks quickly and take corrective action before claims are denied or delayed. Additionally, adopting standardized coding practices can significantly reduce errors during claims submission. Ensuring that coders are well-trained in the latest coding guidelines minimizes discrepancies that could lead to claim rejections.
Furthermore, establishing clear communication channels with payers can expedite the resolution of any issues that arise during the claims process. By proactively addressing potential challenges, healthcare organizations can accelerate revenue generation and improve their overall financial performance.
Optimizing Coding and Documentation for Accurate Billing
Accurate coding and documentation are fundamental to successful Revenue Cycle Management. The coding process translates medical services into billable codes that insurance companies recognize; thus, precision is crucial. Healthcare providers must ensure that their coding staff is well-versed in the latest coding systems, such as ICD-10 and CPT codes.
Regular training sessions and updates on coding changes can help maintain accuracy and compliance. Documentation also plays a vital role in supporting coding accuracy. Comprehensive clinical documentation provides the necessary context for coders to assign appropriate codes confidently.
Healthcare organizations should implement standardized documentation practices to ensure consistency across all providers. By optimizing both coding and documentation processes, organizations can reduce claim denials and enhance revenue capture.
Enhancing Patient Engagement for Timely Payments
Patient engagement is an often-overlooked aspect of Revenue Cycle Management that can significantly impact payment timelines. Engaging patients throughout their healthcare journey fosters transparency and encourages timely payments. One effective strategy is to provide patients with clear information regarding their financial responsibilities before services are rendered.
Additionally, leveraging technology to facilitate patient communication can enhance engagement further. Automated reminders for upcoming appointments or outstanding balances can prompt patients to take action on their financial obligations.
Offering multiple payment options, such as online payments or payment plans, also makes it easier for patients to settle their bills promptly. By prioritizing patient engagement, healthcare organizations can improve collections and reduce days in accounts receivable.
Utilizing Data Analytics to Identify Revenue Opportunities
Data analytics has emerged as a powerful tool for identifying revenue opportunities within Revenue Cycle Management. By analyzing historical data on claims submissions, denials, and payments, healthcare organizations can uncover trends that inform strategic decision-making. For instance, identifying common reasons for claim denials allows organizations to address underlying issues proactively, reducing future revenue loss.
Moreover, predictive analytics can help organizations forecast future revenue streams based on historical patterns and patient demographics. This insight enables providers to allocate resources more effectively and develop targeted strategies for improving collections. By harnessing the power of data analytics, healthcare organizations can make informed decisions that drive revenue growth and enhance overall financial performance.
Addressing Denials and Appeals to Maximize Revenue
Denial management is a critical component of Revenue Cycle Management that requires focused attention to maximize revenue potential. When claims are denied, it is essential to conduct a thorough analysis to understand the reasons behind the denial. Common causes may include incorrect coding, lack of medical necessity documentation, or failure to obtain prior authorization.
By identifying these issues early on, organizations can implement corrective measures to prevent similar denials in the future. Additionally, having a structured appeals process in place is vital for recovering denied claims. This process should involve timely follow-up on denied claims and clear communication with payers regarding the reasons for appeal.
Training staff on effective appeal strategies can significantly improve success rates in overturning denials. By addressing denials proactively and efficiently managing appeals, healthcare organizations can recover lost revenue and strengthen their financial position.
Ensuring Compliance with Regulations and Payer Requirements
Compliance with regulations and payer requirements is paramount in Revenue Cycle Management to avoid costly penalties and ensure smooth operations. Healthcare organizations must stay informed about evolving regulations at both federal and state levels, including those related to billing practices, coding standards, and patient privacy laws such as HIPARegular compliance audits can help identify potential gaps in adherence to these regulations. Furthermore, maintaining open lines of communication with payers is essential for understanding their specific requirements regarding claims submissions and documentation standards.
Establishing strong relationships with payer representatives can facilitate smoother interactions when issues arise. By prioritizing compliance efforts, healthcare organizations can mitigate risks associated with regulatory violations while ensuring timely reimbursement for services rendered.
Training and Education for Staff to Improve RCM Performance
Investing in training and education for staff involved in Revenue Cycle Management is crucial for enhancing overall performance. A well-trained workforce is better equipped to navigate the complexities of medical billing processes, leading to improved accuracy and efficiency. Organizations should prioritize ongoing education programs that cover topics such as coding updates, regulatory changes, and best practices in billing.
Moreover, fostering a culture of continuous learning encourages staff members to stay engaged and motivated in their roles. Providing opportunities for professional development not only enhances individual skills but also contributes to team cohesion and collaboration. By prioritizing training initiatives, healthcare organizations can empower their staff to excel in Revenue Cycle Management and drive positive financial outcomes.
Continuous Monitoring and Improvement of RCM Processes
Continuous monitoring and improvement of Revenue Cycle Management processes are essential for sustaining long-term success in healthcare finance. Organizations should establish key performance indicators (KPIs) to track the effectiveness of their RCM efforts regularly. Metrics such as days in accounts receivable, claim denial rates, and collection ratios provide valuable insights into operational performance.
Additionally, conducting regular reviews of RCM processes allows organizations to identify areas for improvement proactively. Engaging staff in these discussions fosters a culture of accountability and encourages innovative problem-solving approaches. By committing to continuous monitoring and improvement efforts, healthcare organizations can adapt to changing market conditions while optimizing their revenue cycle for sustained financial health.
In conclusion, effective Revenue Cycle Management is vital for the financial sustainability of healthcare organizations. By understanding its intricacies and implementing best practices across various aspects—from patient engagement to compliance—providers can enhance their revenue generation capabilities significantly. Leveraging technology and data analytics further empowers organizations to identify opportunities for growth while addressing challenges such as denials efficiently.
Ultimately, investing in staff training and committing to continuous improvement will ensure that healthcare providers remain resilient in an ever-evolving landscape while maximizing their revenue potential.
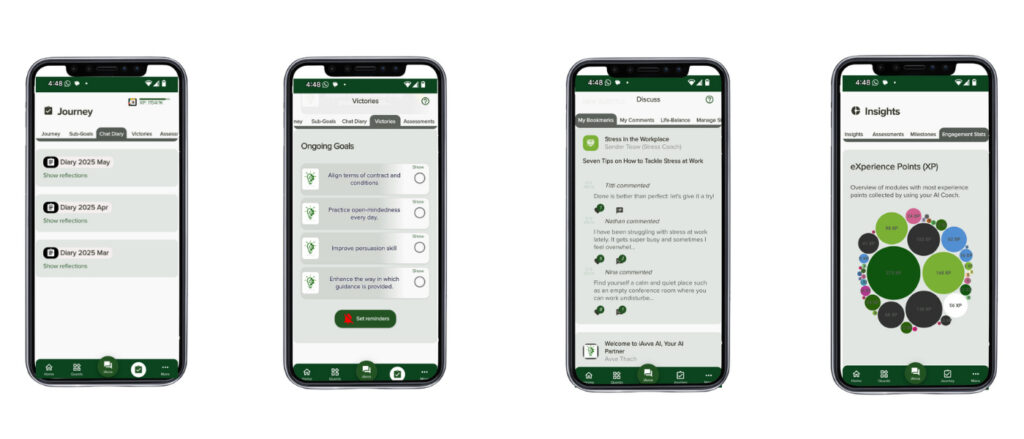
In the realm of medical billing, Revenue Cycle Management (RCM) plays a crucial role in ensuring that healthcare providers receive timely payments for their services. A related article that delves into the transformative potential of technology in business is available at How to Build an AI Strategy That Transforms Your Business. This article discusses how integrating advanced technologies, such as artificial intelligence, can streamline processes and enhance efficiency, which is particularly relevant for optimizing RCM in the healthcare sector.
FAQs
What does RCM stand for in medical billing?
RCM stands for Revenue Cycle Management, which is the process of managing the financial transactions and administrative functions related to patient services in healthcare.
Why is RCM important in medical billing?
RCM is important because it ensures that healthcare providers are properly reimbursed for their services by efficiently managing claims, payments, and patient billing, thereby maintaining the financial health of the practice.
What are the key steps involved in the RCM process?
The key steps in RCM include patient registration, insurance verification, charge capture, claim submission, payment posting, denial management, and patient billing and collections.
Who is responsible for RCM in a healthcare organization?
RCM can be managed by in-house billing staff, dedicated RCM teams, or outsourced to specialized medical billing companies that handle the entire revenue cycle process.
How does RCM impact patient experience?
Effective RCM can improve patient experience by providing clear billing information, reducing billing errors, and offering flexible payment options, which helps minimize confusion and financial stress for patients.
What are common challenges faced in RCM?
Common challenges include claim denials, delayed payments, inaccurate patient information, complex insurance policies, and regulatory compliance issues.
How can technology improve RCM in medical billing?
Technology such as electronic health records (EHR), practice management software, and automated billing systems can streamline workflows, reduce errors, speed up claim processing, and enhance reporting capabilities.
What role does insurance verification play in RCM?
Insurance verification is critical in RCM as it confirms patient coverage and benefits before services are rendered, reducing the risk of claim denials and ensuring accurate billing.
Can RCM help reduce claim denials?
Yes, by implementing thorough verification, accurate coding, and timely follow-up on claims, RCM processes can significantly reduce the frequency of claim denials.
Is RCM only applicable to hospitals?
No, RCM is applicable to all healthcare providers including hospitals, clinics, physician practices, and other medical facilities that bill for patient services.





Leave a Reply